Access: The TAC Blog
News, Resources, & Happenings at TAC: February 2020
Beyond Pizza — How Communities Handle Compensation and other Practical Issues with Young Adult Partners
Communities working to end youth homelessness are increasingly bringing youth and young adults with lived experience of homelessness to the forefront of their planning and implementation efforts, often with the support of a HUD Youth Homelessness Demonstration Program award. Of course, the young people who contribute their energy and insights should be compensated for their time - but how, and how much? TAC Senior Associate Lauren Knott, together with consultant Lauren Leonardis, surveyed a range of Youth Action Boards (YABs) to find out how they handle this and other challenges. The results are available as The Gab on YABs, a collection of community fact sheets and topic spotlights full of useful information for any community committed to fully incorporating youth and young adult leadership.
Tools for Successful State Partnerships between Medicaid and Housing Agencies
From 2016 to 2018, sixteen states participated in a Centers for Medicare and Medicaid Services (CMS) Innovation Accelerator Program (IAP) State Medicaid-Housing Agency Partnerships track. The tools developed and used to provide technical assistance to these states, incorporating the work and expertise of many TAC colleagues, form the basis of a new State Medicaid-Housing Agency Partnerships Toolkit published recently to the LTSS website. The toolkit is designed to assist states as they consider systems-level changes that further community integration, including the intersection between health care and housing. It is available for states to download, use, and adapt.
Trainings for Trainers in a Unique Rapid Resolution Pilot Program for Veterans
TAC has recently hosted several three-day events focused on homelessness diversion and rapid exit strategies for Veterans. These "train the trainers" sessions, conducted in partnership with the Cleveland Mediation Center and Abt Associates, are part of our support for the Department of Veterans Affairs' Supportive Services for Veteran Families (SSVF) program. Over the past two years, TAC and our partners have provided a wide range of onsite, remote, and training technical assistance in the development and rollout of SSVF's "Rapid Resolution" initiative, the first nationwide federal effort of its kind - a pilot program that supports diversion strategies for Veterans who are entering homelessness or have only recently become homeless. The recent trainings teach critical diversion and rapid exit skills in the context of SSVF's program design and implementation, with an emphasis on giving practitioners the tools they need to transfer that knowledge to their home communities. The training effort is led by TAC Senior Associate Douglas Tetrault, with strong support from other TAC staff members and TAC partners, and project direction from TAC Senior Consultant Jim Yates.
STAFF ACTIVITIES
TAC staff members Jenna Espinosa, Ellen Fitzpatrick, Ayana Gonzalez, Lauren Knott, & Ashley Mann-McLellan have been facilitating convenings and providing TA for Youth Homelessness Demonstration Program communities in Iowa, New York, Massachusetts, and Maine; Associate Ellen Fitzpatrick and Senior Associate Ashley Mann-McLellan conducted a 3-part training for Boston agency directors to strengthen the role of housing navigators in their organizations, and is helping the Boston Public Health Commission with a strategic plan to make its 800-bed shelter more housing-focused; Ashley was also one of 350 volunteers in Boston's 40th annual homeless census - thanks, Ashley! Senior Associate Melany Mondello led a training for the Vermont Balance of State Continuum of Care on the definition and documentation standards of chronic homelessness; Senior Consultant John O'Brien spoke about the future of policy and payment at a Substance Use Disorder Action Forum hosted by the Medicaid Transformation Project; Senior Associate Rachel Post facilitated the first cohort of Housing and Healthy Communities Learning Network, with plans for a second round in the works; Senior Associate Tyler Sadwith launched a provider-to-provider pilot program to test an approach for delivering TA on medication-assisted treatment to California's Tribal health programs; and Tyler also joined Senior Consultant John O'Brien to share strategic planning advice at a roundtable for Pew Charitable Trust's Substance Use Prevention and Treatment initiative.
STAFF TRANSITIONS
TAC is growing! A warm welcome to Project Support Specialists Laura Harris and Ari Rogers; Communications Designer Jeff Nguyen; Associates Eric Gammons and Jenna Espinosa in our housing group; and Dayana Simons and David de Voursney, two new Senior Consultants in our human services group. Learn more about our new colleagues on the TAC staff page.
News, Resources, & Happenings at TAC: June 2019
Challenges and Solutions in Rural Mental Health
Q: What are the most important steps to improve mental health in the rural United States? A: Access to care, insurance coverage, and strong social determinants - like affordable housing - that can reduce need. In recognition of Mental Health Month, TAC Executive Director Kevin Martone discussed these topics recently with Beth O'Connor, director of the Virginia Rural Health Association, on her Rural Health Voice podcast (episode #16).
Expanding Access to Substance Use Disorder Treatment through Medicaid
The TAC Human Services team is engaged in efforts to support states in addressing substance use disorder (SUD) needs through their Medicaid programs.
In April, with support from Arnold Ventures, TAC published a brief on State Approaches to Developing the Residential Treatment Continuum for Substance Use Disorders. This resource offers valuable peer insights to help state Medicaid agencies in their efforts to incorporate residential SUD treatment providers into Medicaid provider networks. TAC Senior Consultant John O'Brien, Senior Associate Tyler Sadwith, and co-authors focus on five states that have been early leaders in modernizing their SUD treatment systems: California, Maryland, Massachusetts, Michigan, and Virginia. Drawing on interviews with leaders in these states, the brief identifies key decision points that other states are likely to encounter as they too expand coverage for residential SUD treatment services. Strategic recommendations based on the experiences of these five leading states are offered; best practices highlighted; and factors identified that states should consider when implementing section 1115 SUD demonstration projects and other SUD program reforms.
TAC followed up publication with a webinar to present the major findings in the brief, focusing especially on key decision points and recommendations for state Medicaid agencies. Medicaid leaders from Maryland and Virginia were featured presenters, explaining critical steps they have taken to engage their SUD residential provider communities and provide access to evidence-based practices such as medication-assisted treatment.
In early and mid-May, with support from Arnold Ventures, TAC kicked off engagements with Ohio, Louisiana, and West Virginia. TAC's technical assistance will help these states in their efforts to improve access to high-quality medication-assisted treatment for opioid use disorder through targeted transformation initiatives. TAC consultants and partners met with key officials from Medicaid, substance abuse agencies, and managed care organizations - as well as patient advocates and pharmacy stakeholders - to discuss priority focus areas and options in the design, development, and implementation of interventions.
TAC Staff in Action
Staff Activities
TAC Associate Ashley Mann-McLellan presented on "Homelessness Solutions: Housing-Focused Outreach" at the Louisiana Housing Conference in Baton Rouge; TAC consultant Naomi Sweitzer attended the spring conference of the Southwestern Affordable Housing Management Association, where she co-presented with with HUD, Austin (TX) ECHO, and Prak Property Management on the Multifamily Homeless Preference.
August 2017: News, Resources, and Happenings at TAC
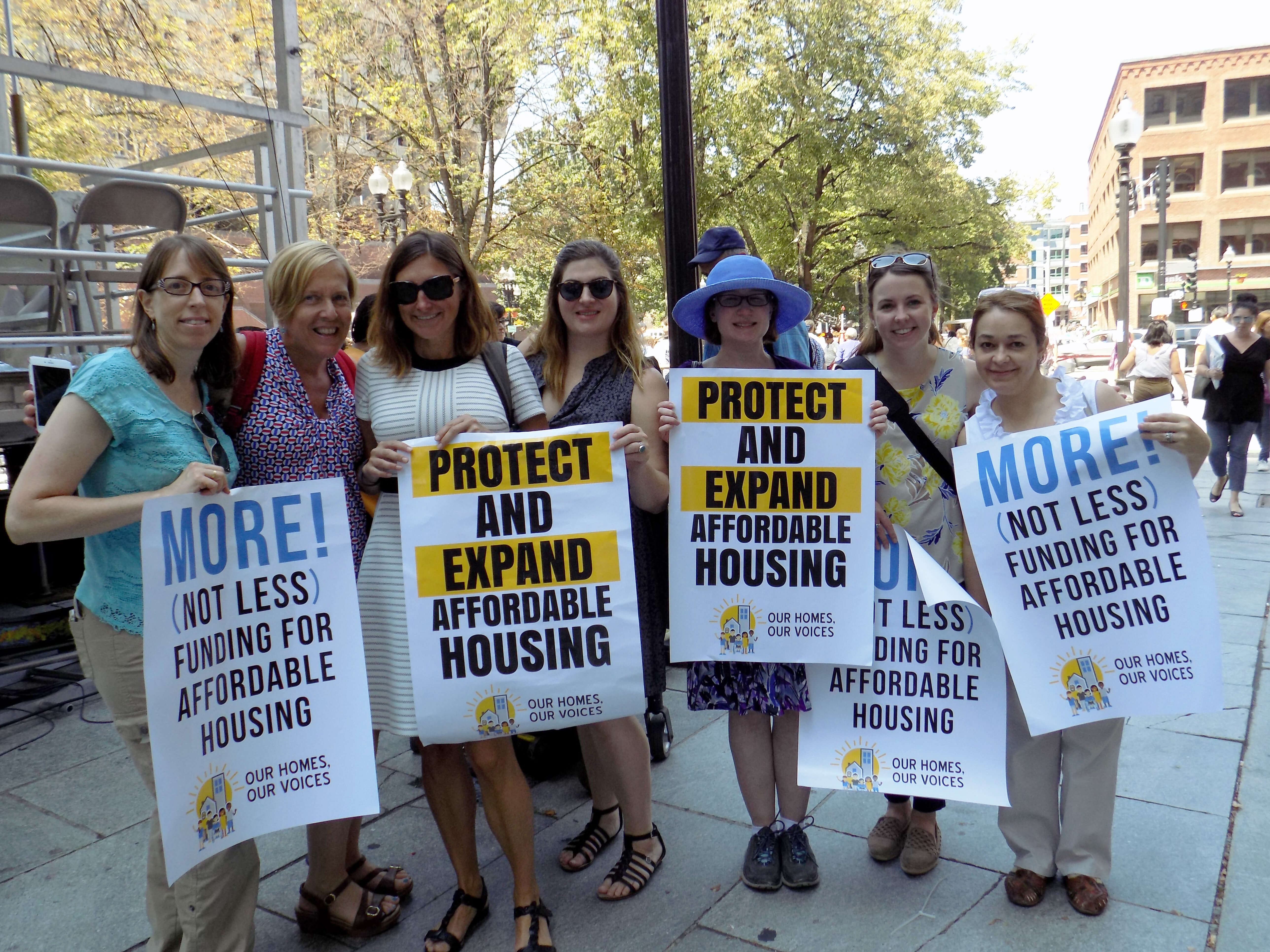
Our Homes, Our Voices — No Housing Cuts!
TAC staff headed over to historic Faneuil Hall a few weeks ago, where we joined hundreds of other housing and disability rights advocates, subsidized housing residents, and community leaders to tell the federal government: NO CUTS TO HOUSING! The Boston rally was organized by our friends at the Citizens' Housing and Planning Association in coordination with events held around the country. Check out our Facebook photo album to see a few of the speakers we cheered for, and take a look at #OurHomesOurVoices on Twitter for a national snapshot.
New Action Plan Launched for Permanent Supportive Housing in North Carolina
Many of the strategies in North Carolina's 2017 Permanent Supportive Housing Action Plan are based on a Permanent Supportive Housing Assessment with Recommendations to Comply with the Olmstead Settlement produced by TAC. The shared vision for permanent supportive housing in North Carolina connects people to affordable, integrated, and supportive housing by leveraging resources and collaborating with all levels of government and private agencies.
CMS Helps States to Foster Community Living Opportunities
The Centers for Medicare and Medicaid Services (CMS) has announced a second round of the State Medicaid-Housing Agency Partnerships track in its Medicaid Innovation Accelerator Program (IAP). The goals of this track are to develop public and private partnerships between state Medicaid and housing systems and to support states in creating detailed action plans that foster community living opportunities for Medicaid beneficiaries. TAC is part of the IAP technical support team that will work from August 2017 through April 2018 with eight states: Alaska, Massachusetts, Michigan, Minnesota, Nebraska, Texas, Utah, and Virginia. Visit the CMS website to learn more.
TAC Staff in Action
STAFF ACTIVITIES
TAC Associates Phillip Allen, Ellen Fitzpatrick, and Ashley Mann-McLellan and Senior Associate Melany Mondello attended the National Conference on Ending Homelessness in Washington, D.C. last month, with presentations by Phil on the SSVF System Assessment Toolkit and by Ashley on the intersection of housing, mental health, and substance abuse; Jon Delman, Senior Associate, was an invited participant in SAMHSA's expert resource meeting on "Advancing Behavioral Health Treatment & Recovery through Technology" and led a workshop on "Fighting for our Livelihoods: Developing Job Opportunities for Economic Self-Sufficiency" at the National Empowerment Center's Alternatives Conference; Associate Lauren Knott and other experts helped out at a forum for SAMHSA's 10 Youth Homelessness Demonstration communities; Executive Director Kevin Martone described the importance of affordable housing for people with disabilities at a #NoHousingCuts Congressional reception organized by Monarch Housing Associates of New Jersey; Kevin also spoke on the role of community-based mental health services and housing in reducing reliance on emergency and inpatient care in his address to mental health authority leaders gathered at the National Association of State Mental Health Program Directors' annual conference; and Senior Consultant Jim Yates was promoted to the rank of Colonel in the Army National Guard - congratulations, Jim!
STAFF TRANSITIONS
We are happy to welcome Hawo Osman as a TAC intern this summer. Hawo is a rising senior at Medford High school and joins us through the Boston Center for Independent Living’s Transition Internship Program.
July 2017: News, Resources, and Happenings at TAC
TAC Scholarship Helps Launch a Teacher, a Social Worker, a Nurse, and a Chef
We are delighted to introduce this year’s recipients of the second annual Day-O'Hara Community Integration Scholarship. This cash award, given in honor of TAC co-founders Steve Day and Ann O'Hara, is intended to help individuals with disabilities in the Greater Boston area to realize their educational and professional goals.
Eddie Shields is currently employed as a teacher’s assistant and was referred to us through the Boston Center for Independent Living. He will use the scholarship money towards courses to obtain his Associate’s Degree in early childhood education.
Kayla Wilson is a Long-term Support Services Coordinator at the Boston Center for Independent Living. Kayla has discovered that her true passion is to assist individuals from both the medical and social points of view simultaneously, and plans to use the scholarship money towards prerequisite courses for nursing programs.
For two years, Lisa Jones has volunteered weekly to serve meals to elders in need. Lisa was referred to us by the Transformation Center, and will use the scholarship money for a post-bachelors program in gerontology — moving her closer to her goal of attaining a Master’s degree in social work or human services so that she can work in a wraparound program to help elders stay in their own homes.
Silvaria DeSilva has a background in nursing, but has recently discovered a love for cooking. She recently graduated from Pine Street Inn’s food service training program, and will use the scholarship money for cooking classes and to buy the supplies and materials she’ll need as a professional chef or caterer.
Best of luck to all, and thanks to the partner organizations that helped us connect with these inspiring individuals!
Successfully Employing and Financing Peer Specialists in Behavioral Health
The inclusion of peer providers on behavioral health care teams can significantly improve client engagement and outcomes, including symptom reduction, improved self-esteem, and community integration. Yet behavioral health providers sometimes struggle to maintain a strong peer workforce — leading to diminished productivity and increased stress for all staff. In TAC’s new training for behavioral health providers, managed care organizations, and state/county behavioral health authorities, participants will learn how to introduce appropriate supports and key shifts in workplace culture to promote both peer job success and stronger organizations overall.
TAC Staff in Action
Staff Activities
In June, Managing Director Marie Herb and Senior Associate Gina Schaak served as volunteer “Ambassadors” at Boston’s Third Surge to End Chronic Homelessness (read all about it!); TAC Associate Ashley Mann-McLellan presented on “Using Data to Improve Outcomes and HUD’s System Performance Measures” at the All Home Annual Conference in Seattle, WA; Kevin Martone, Executive Director, recorded a webinar for Foothold Technology on "Navigating the World of Medicaid for Supportive Housing Services"; and at the National Coalition for Homeless Veterans conference, TAC Associate Douglas Tetrault co-presented with our partners from Abt Associates on how to assess the components of a crisis response system and develop improvement strategies.
February 2017: Can States Take On the Fiscal Responsibility that Federal Policymakers Are About to Hand Them?
A FEW WEEKS AGO, I had the opportunity to explain to a roomful of congressional staffers the profound impact that a repeal of Medicaid expansion would have on individuals with substance use disorders - and on the systems that serve them. In the questions that followed, an underlying theme was evident: Would lost Medicaid revenue and other federal resources be replaced by state funds to pay for such services? This issue has far-reaching implications for all of our nation's safety net programs. Both my current work with state systems across the country and my experience as a former state commissioner of behavioral health make clear to me that states are in no position to absorb the transfer of fiscal responsibility they are about to receive from federal policymakers.
Systems Work Better Together
In every state, there are vulnerable populations whose complex challenges require coordinated solutions that use federal and state funding. In recent years, awareness has grown in both the health care and affordable housing communities of the positive outcomes to be attained by leveraging these resources together. State Medicaid directors have become educated on the costs to their programs of individuals with chronic health conditions who are homeless, at risk of homelessness, or living in substandard housing. Likewise, affordable housing leaders have learned that lack of access to health insurance, and especially to integrated behavioral and primary health care services, jeopardizes housing stability. States are becoming sophisticated in their use of interventions that build on this new understanding, such as supportive housing - an approach that combines affordable housing assistance with wraparound supportive services. Such states have increasingly demonstrated cost savings in their systems.
The availability of federal funding has afforded states the opportunity to improve the lives of millions of children and adults. The option to expand Medicaid through the Affordable Care Act (ACA) allowed states to increase access to care for populations with many health needs, create better health care delivery systems, and save taxpayer dollars. Federal funding was the incentive needed for 31 states and the District of Columbia to expand coverage, while states that did not expand Medicaid still rely on significant federal support to operate their traditional Medicaid programs. Federal housing assistance programs have been a critical resource for millions of seniors, people with disabilities, and people living on very little income - though a significant gap remains between available assistance and need.
Shifting the Burden to States
The imminent repeal of Medicaid expansion and the ACA, and proposals to convert Medicaid to a block grant or per capita program, threaten millions of people's access to health care, with disproportionate consequences for vulnerable populations. While these changes will create significant savings for the federal government, states will in turn experience both immediate and long-term pressures to fill the void - allegedly in exchange for more control and "flexibility." Under a block grant plan previously proposed by former House Budget Chair and Health and Human Services Secretary nominee Tom Price, the Medicaid and Children's Health Insurance Program would receive 34 percent less funding in 2025 than under the current federal law.
Decreases in affordable housing assistance resulting from cuts to non-defense discretionary (NDD) programs like those at HUD will disproportionately affect the same populations impacted by cuts in Medicaid. We don't have to look too far back to see how this plays out: the March 2013 sequestration cuts forced state and local housing agencies to decrease the number of households using tenant-based vouchers by more than 80,000. About half of all voucher recipients are seniors or people with disabilities, most of whom live on fixed incomes such as Social Security or Supplemental Security Income (SSI) and rely on Medicaid. In not a single rental housing market in the country can a person with a disability who is living on SSI afford housing at the "fair market rent" determined by HUD. According to the National Low Income Housing Coalition, the United States has a shortage of 7.2 million rental units affordable to extremely low-income renter households. Yet President Trump has proposed a one-percent reduction to NDD each year for the next ten years. Even a simple freeze, suggested by several members of Congress, would result in the defunding of housing vouchers currently used by more than 100,000 families in 2017 alone.
Faced with such a significant loss of federal support, Democratic and Republican governors, legislators, and mayors will have to make some very difficult budgetary decisions. Will these leaders, as many have suggested, find ways to sustain access to health benefits, affordable housing assistance, and social services once federal policymakers shift the financial burden onto states?
Hard Choices
Recent history shows that as resources are squeezed, many states are unable or unwilling to prioritize vulnerable populations. Most Medicaid expansion states were in a position to increase coverage only because of significant federal matching. Without such support, states have generally opted to provide only limited benefits to people who are traditionally ineligible for Medicaid, and several states have established highly restrictive eligibility criteria. Economic downturns can create added challenges for states as tax revenues decrease while unemployment and enrollment in Medicaid increase. According to the U.S. Government Accountability Office (GAO), during the nation’s last recession, Medicaid enrollment grew by 14.2 percent from October 2007 through February 2010. During the same period, total Medicaid expenditures grew nearly 21 percent, from $332.2 billion in 2007 to $401.5 billion in 2010.
To reduce program spending, the GAO noted, states generally make certain changes to their Medicaid programs, such as altering payments to providers, limiting eligibility, eliminating optional services, or reducing the amount, duration, or scope of services covered. Even as need rose, states cut funding for a range of services by 4.2 percent in fiscal year 2009 and an additional 6.8 percent in 2010, according to estimates by the National Association of State Budget Officers (NASBO). In 2011, two-thirds of states cut provider payments, and 18 states reduced Medicaid benefits. The recession of 2009–2012 resulted in losses of over $4 billion from public behavioral health systems across the country, losses from which they have still not fully recovered.
Most states have allocated resources to support housing assistance for low-income populations. A report prepared by the Technical Assistance Collaborative in 2014 indicated that 34 states offer some type of rental assistance or homelessness prevention funds (e.g. security deposits). However, there is wide variation in the number of individuals such programs can support, and program funding tends to fluctuate annually due to state budget pressures. Indeed, a NASBO survey conducted in the fall of 2016 indicated that in 24 states, general fund revenues for 2017 are coming in below projections, the greatest number of states expecting revenue shortfalls at this time in the fiscal year since 2010. Nineteen states reported net mid-year budget reductions in fiscal 2016, a historically high number outside of a recession period.
There is indisputable evidence that the availability of health insurance and access to health care and affordable housing improve people's lives. As lawmakers contemplate dramatic reductions that will hurt people and economically burden states, we find ourselves at a pivotal point. There is little evidence to suggest that state governments can or will assume the financial responsibility offloaded by the federal government under current proposals. Yet, it is state and local budgets that must absorb the preventable economic consequences when individuals engage costly, crisis-oriented health care, correctional, and homelessness systems. Federal policymakers must understand that a cost shift to states under the guise of flexibility and efficiency will have dramatic and unfortunate consequences for vulnerable individuals and their families.