Access: The TAC Blog
December 2017: Affordable Housing for People with Disabilities
The tenth edition of the Priced Out: The Housing Crisis for People with Disabilities report, released today by TAC and our partners at the Consortium for Citizens with Disabilities Housing Task Force, once again demonstrates that non-elderly adults with disabilities who rely on Supplemental Security Income (SSI) are among the groups most severely affected by the extreme shortage of affordable rental housing across our nation.
Over the last decade, increased rental demand combined with development primarily at the high end of the market has led to record-low vacancy rates, higher rents, and increased competition for affordable and subsidized housing. This overall market trend is reflected in the ever-worsening affordability gap for extremely low-income renters with disabilities.
Supplemental Security Income is the federal income maintenance program that assists people with significant and long-term disabilities who have virtually no assets and — in most instances — no other source of income. The national average rent for a studio/efficiency unit in 2016 was $752, equal to 99% of a monthly SSI payment. In thirteen states and the District of Columbia, areas with the highest housing costs in the nation, the average studio/efficiency rent exceeded 100% of the income of an SSI recipient.
This housing affordability crisis deprives hundreds of thousands of people with disabilities of a basic human need: a place of their own to call home. Because of the disparity between SSI income and rental housing costs, non-elderly adults with significant disabilities in our nation are often forced into homelessness or segregated, restrictive, and costly institutional settings such as psychiatric hospitals, adult care homes, nursing homes, or jails.
Ideally, there would be enough job opportunities that match the skills of people with disabilities and pay a livable wage so that all could afford housing in their communities. However, as the National Low Income Housing Coalition documents in its 2017 Out of Reach report, it would require more than two full-time jobs at the federal minimum wage to pay for a one-bedroom apartment at fair market rent.
Federal rental assistance — meaning a subsidy that helps renters pay no more than 30% of their income for housing — is the key to solving the housing crisis that has been documented in Priced Out reports over the past 19 years. Unfortunately, because of funding limitations that have grown worse in recent years, federal rental subsidy programs currently reach only 35 of every 100 extremely low-income households; with incomes equal to only 20% of area median income, one-person households receiving SSI fall within this category. This shortfall translates into long waiting lists at Public Housing Agencies and affordable housing developments, and a critical shortage of permanent supportive housing opportunities for people with significant disabilities who have SSI-level incomes.
A unified advocacy effort by the disability community is needed to support and potentially expand permanent supportive housing programs along with other rental assistance strategies. Providing housing assistance to people with the most significant and long-term disabilities is not only the right thing to do, but is also more cost-effective than perpetuating the alternatives: costly institutional care, uncontrolled expenses to the health care system, and homelessness.
December 2017: Coordinated Entry — What's Working Well
FOR SEVERAL YEARS, TAC consultants have been on a journey with communities to create effective, sound Coordinated Entry (CE) systems and processes that contribute to their larger goal of ending homelessness. As the U.S. Department of Housing and Urban Development’s (HUD) January 23, 2018 deadline for Coordinated Entry compliance nears, we want to share some planning tips that we have seen contribute to creative and efficient systems.
Align Your Local Goals to End Homelessness WITH HUD’s Goals for Coordinated Entry
We often see communities concerned about the compliance aspect of Coordinated Entry, which leads them to direct planning efforts toward the goal of “checking off the boxes” of Coordinated Entry requirements. We challenge communities instead to consider Coordinated Entry a powerful tool in their efforts to end homelessness. HUD promotes some key strategies that really are essential in reducing and ending homelessness, such as ensuring that all processes are as low-barrier as possible, implementing uniform assessment to ensure uniform decision-making across systems, and prioritizing assistance to the most vulnerable. Some planning activities to align your own local goals with the goals of Coordinated Entry might be helpful:
-
Create a crosswalk between key goals in your local strategic plan to end homelessness and those in HUD’s Coordinated Entry Notice.
-
Spend some time with your stakeholders envisioning your ideal system for any consumer. Draw on this process to create a list of values that will guide decision-making throughout the CE planning process.
-
Engage local funders to be part of planning efforts by finding alignment between their goals and your CE goals.
Integrate Change Management Strategies into Planning
Implementing Coordinated Entry is a significant systems change, and will continue to have effects long past a community’s first iteration of CE. It is important to acknowledge the shift that stakeholders will undergo, and to use change management strategies that can strengthen the planning process:
-
Continually acknowledge the change that is happening. This will start to normalize the process, making the reality of systems change familiar to your stakeholders.
-
Engage your stakeholders in creating the system, or in problem-solving any challenges that arise. People often respond better to change if they are part of the thought process, rather than having change forced upon them.
-
Work to create a culture of innovation and “failing forward.” It’s good to make use of reference materials to guide Coordinated Entry planning processes, but the bottom line is that there is no pre-packaged Coordinated Entry system with assembly instructions. Each community must figure out what works given its own local stakeholders, populations, and conditions. A learning culture that celebrates innovation can help to promote new ideas and reduce negative backlash toward methods that were tried but did not succeed. We are seeing this type of culture work well particularly in the development of diversion techniques within Coordinated Entry.
Promote Fidelity to Housing First
The guiding principles of the Housing First philosophy are critical to creating flow through your Coordinated Entry system. Practices such as lowering barriers to housing admission, creating housing pathways and processes with a commitment to referral success, fostering participant choice, prioritizing assistance to the most vulnerable, and terminating participants from housing programs only in the most egregious cases not only create system flow, but also poise communities to improve their success in several of HUD’s system performance measures. To maintain fidelity to Housing First, there are several actions your community can take:
-
Incorporate consumers into your planning process. Communities have found many ways to infuse consumer voices into planning in a meaningful way. Often the key is to employ several strategies at once: hold multiple seats for consumers on your planning committees and Continuum of Care board; create a consumer advisory body to receive an even more diverse set of viewpoints; hold focus groups with consumers who may not be able to commit to an ongoing committee, but who would like to give input; and compensate consumers for their time.
-
Continually assess programs’ fidelity to Housing First. Programs may incorporate self-assessments, such as the Housing First Assessment recently released by HUD, to gauge current fidelity and identify areas for improvement. Many communities have also found success in setting up learning collaboratives for both frontline and manager-level program staff to share strategies in implementing a Housing First philosophy.
-
Get funders trained and engaged in Housing First. At TAC, we have done substantial work with communities’ funders to assist them in aligning their contracts, performance targets, and monitoring processes with the Housing First philosophy. Getting funders on board helps with the promotion of Housing First not only at a program level, but at a systems level.
We are continually impressed by the perseverance we have seen in communities to create Coordinated Entry systems and processes that can drive progress towards ending homelessness. We look forward to continuing to learn alongside you!
November 2017: Will Opening Up More Psych Beds Really Address the Opioid Crisis? Not So Fast.
The Trump administration’s interest in addressing the opioid epidemic is heartening, and last week's proclamation is a welcome acknowledgment that opioid addiction and overdoses do indeed constitute a major public health crisis in our nation. While there is no immediate prospect of a significant cash infusion (millions are touted, versus the badly needed billions) to address the crisis, there has at least been the promise of statutory and regulatory relief — with a particular focus on allowing states to waive the Institutions for Mental Diseases exclusion. This 52-year-old statute bars Medicaid payments for mental health and addiction treatment provided to individuals in large treatment facilities, and some advocates assert that waiving it will allow Medicaid funds to flow for thousands of substance use disorder (SUD) treatment beds that currently lie empty.
All efforts to expand access to treatment are important, but the push to open up large facilities for SUD care as the first priority should be kept in perspective. Empty beds in such institutions may be the result of many causes. For instance, a community with a strong array of community-based treatment options may not need additional beds. In some cases, beds go unused if private payers don't refer patients to a facility because it lacks a modern, evidence-based approach to treating addiction (for instance, if no-one on staff is qualified to provide medication-assisted treatment). And finally, some facilities have never participated in either Medicaid or commercial insurance programs simply because they don’t have to, as their private fee structure allows them to maintain empty beds; these providers may have neither the financial motivation nor the business operations know-how to bill insurers, or to train their staff to meet the quality standards of states and commercial payers.
So, states — before you rush off to the Centers for Medicare and Medicaid Services asking for IMD waivers, make sure your request is going to make a true difference in getting people high-quality care. We won’t turn this crisis around by assuming that any treatment is better than no treatment.
November 2017: Putting Psychiatric Hospitalization into Context
THE NUMBER OF STATE INSTITUTIONAL PSYCHIATRIC BEDS, which were once the primary setting for psychiatric treatment, has gone down dramatically nationwide. Community psychiatric hospitals, private hospitals, and nursing facilities filled the gap in the 1980s and '90s, but inpatient capacity in these settings, too, has recently been on the decline. There is widespread concern — given ample voice by the media — that we need to restore our nation’s psychiatric bed capacity, both to reduce the risk of violence perpetrated by people with untreated mental illness, and for their own safety and health.
In reality, however, inpatient treatment should form only one part of a robust system of mental health care. For comparison, note that treatment for even the most serious medical conditions now frequently occurs in outpatient and in-home settings. However, recent findings from the Healthcare Cost and Utilization Project reveal a widening gap between our country’s approaches to hospitalization for mental and for physical health conditions: Between 2005 and 2014, the rate of inpatient stays per 100,000 people for all causes decreased across all age groups, while the number of hospital stays for mental health/substance use actually increased by 12.2 percent.
To examine these trends and their implications, the National Association of State Mental Health Program Directors recently commissioned a series of working papers on the question: “What is the real need for inpatient psychiatric beds in the context of a best practice continuum of care?” In this series, researchers and policy leaders describe ways to improve mental health and substance use disorder treatment at many different points in a community’s system of care so as to necessitate fewer psychiatric hospitalizations, of shorter duration, with better and more equitable outcomes.
Increasing the number of psychiatric inpatient beds is not the solution in most communities. As my colleague Kevin Martone and I argue in our contributions to the series, investments in care and services can create alternatives to inpatient beds that are both more effective and less costly. “Beyond Beds: The Vital Role of a Full Continuum of Psychiatric Care” lays out specific public policy recommendations to minimize the human and economic costs associated with severe mental illness by building and invigorating a robust, interconnected, and evidence-based system of care. And as “The Role of Permanent Supportive Housing in Determining Psychiatric Inpatient Bed Capacity” shows, stable and affordable housing combined with voluntary services can contribute to improved outcomes in both physical and behavioral health, while reducing incarceration and homelessness. Furthermore, the cost of serving a person in supportive housing is half that of a shelter, a quarter that of incarceration, and one-tenth the cost of a state psychiatric hospital bed.
Advances in medical research and technology, chronic disease management programs, and alternative treatment settings such as walk-in urgent care centers — along with payment approaches that support medical care in outpatient settings — have all helped reduce hospitalizations for physical health conditions. Evidence-based mental health care options, especially when provided in the communities where people live, offer the potential to bring down psychiatric hospitalizations as well. Private insurers rarely cover these services, however, and state and federal mental health funding are drastically insufficient to meet demand. Medicare and Medicaid together fund approximately 60 percent of inpatient care in the United States. Unfortunately, Medicare funds very few evidence-based mental health practices, and Medicaid funding for housing transition and tenancy-sustaining programs — a critical component of permanent supportive housing for people with mental health disabilities — is not yet fully incorporated into services.
We don’t need to re-create massive numbers of psychiatric inpatient beds. Rather, policymakers must prioritize funding for the evidence-based preventive treatment and services that people with mental illness need and desire. With these effective and cost-saving resources available and truly accessible in every community, hospitalization will play an appropriate role in a balanced system.
November 2017: News, Resources, & Happenings at TAC
Providers Gather to Focus on Rapid Re-Housing
At the end of October, 800 service providers and Continuum of Care leaders focused on making rapid re-housing (RRH) a key component in their efforts to prevent and end homelessness came together for two intensive days of workshops, presentations, and teamwork. Two Rapid Re-Housing Institutes were held a few days apart in Duluth, GA and Los Angeles, CA, coordinated by TAC in partnership with the Department of Veterans Affairs' Supportive Services for Veteran Families program, the Department of Housing and Urban Development, Abt Associates, the National Alliance to End Homelessness, and the National Coalition for Homeless Veterans. The U.S. Interagency Council on Homelessness and the Department of Labor were also represented at the Institutes.
At each gathering, a Practice Track offered service practitioners direct training in the core components of RRH and effective service delivery strategies. Concurrently, a System Track designed for leaders with planning and implementation responsibilities covered community-wide practices relevant to RRH as a primary response to homelessness. Along with working sessions, Nan Roman, president and CEO of the National Alliance, and Elisha Harig-Blaine, Principal Housing Associate for the National League of Cities, gave plenary addresses - and for a little extra fun, groups competed in rapid re-housing Mad Libs and bingo! For more highlights, check out #RRHI2017.
TAC Staff in Action
Staff Activities
Senior Policy Advisor Francine Arienti and Senior Associate Gina Schaak traveled to Hickory, NC to train providers on assessing people's needs and preferences before helping them move into supportive housing; Senior Associate Jon Delman presented on "Improving Work Conditions for Peer Specialists" at the annual gathering of the International Association of Peer Supporters; Jon also joined Associate Jenn Ingles, Senior Associate Melany Mondello, and Senior Consultants John O'Brien and Jim Yates in Montgomery, AL to help launch a statewide strategic housing initiative; In October, Managing Director Marie Herb and consultant Jake Mihalak facilitated the first on-site meeting of the Violence Against Women Act - Housing Opportunities for Persons With AIDS (VAWA-HOPWA) Demonstration Program initiative; Senior Consultant Sherry Lerch presented to the National Coalition of State Housing Agencies on "The Supportive Housing/Health Care Nexus"; Executive Director Kevin Martone brought a national perspective to a recent article in Mental Health Weekly on New York state's efforts to fund supportive housing; Senior Consultant John O'Brien gave the opening presentation at the National Dialogues on Behavioral Health conference, and spoke on "Strategies for Outcomes and Value-Based Payment" at an American Public Health Association roundtable on systems transformation; and Associates Phillip Allen, Lauren Knott, Ashley Mann-McLellan, and Douglas Tetrault, Senior Associates Melany Mondello, Gina Schaak, and Liz Stewart, consultant Naomi Sweitzer, TA & Training Coordinator Kyia Watkins, Federal Contracts Assistant Kim Wilder, and Housing Intern Madison Tallant all hit the road to put on the first Rapid Re-Housing Institutes in Duluth, GA and Los Angeles, CA (see above).
September 2017: News, Resources, & Happenings at TAC
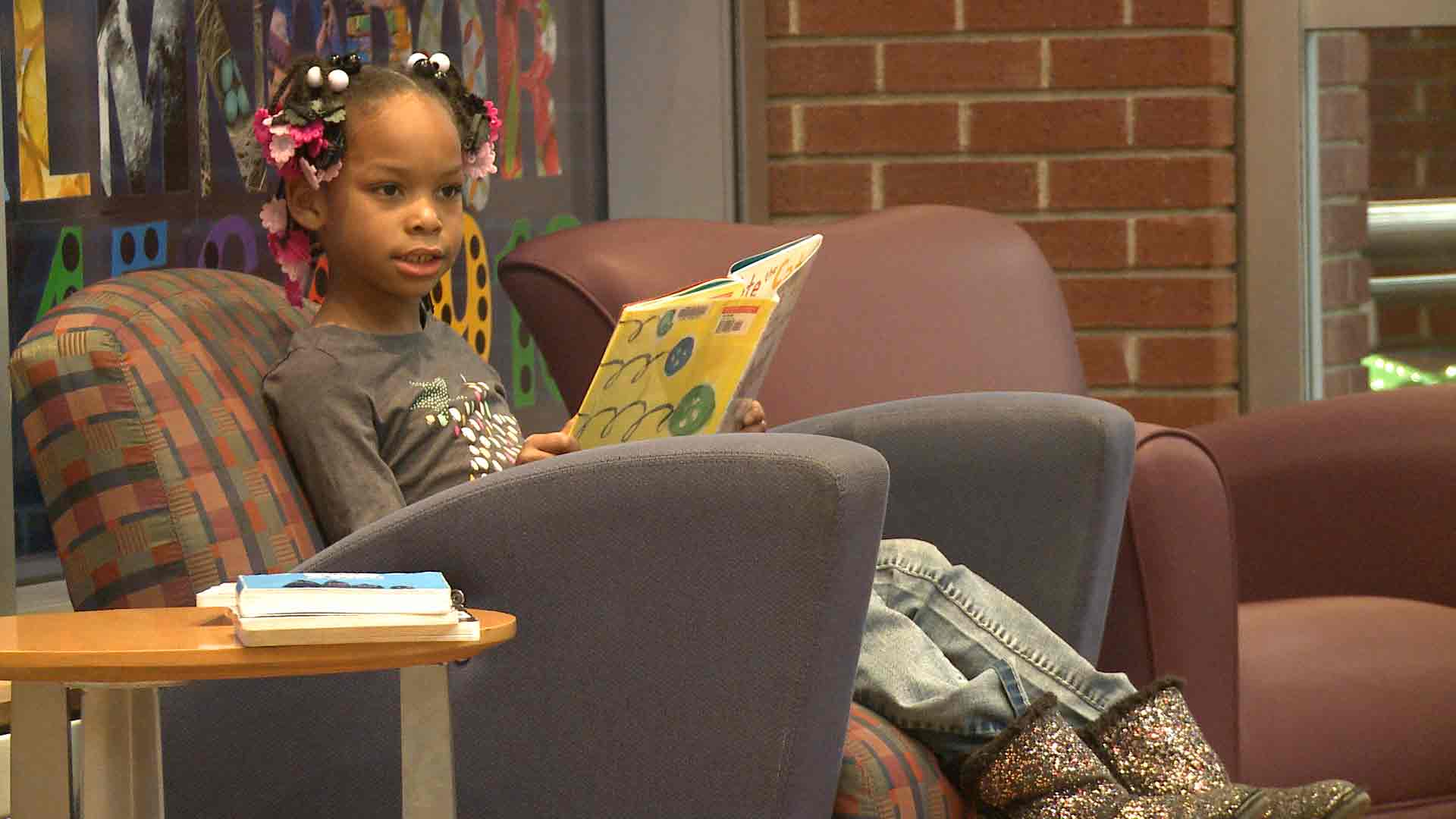
“It Makes Me Feel Like I Mean Something”: Success Stories in Community Integration
Permanent supportive housing enables many people with disabilities to live independently and participate fully in their families and communities. The Section 811 Project Rental Assistance program of the Department of Housing and Urban Development (HUD) helps communities forge partnerships and leverage resources to help people move out of unnecessarily restrictive environments and into their own apartments - and to help them thrive once there. In these videos and vignettes produced by the HUD Office of Multifamily Housing with TAC's assistance, you'll see how community integration through supportive housing looks for Tanesha, Destiny, Avia, and Mr. Poole, four individuals with diverse needs and histories who live in different parts of the country. You will also hear from service providers and property managers about what makes the 811 PRA program work.
Determining the Real Need for Inpatient Psychiatric Beds
Two TAC authors have contributed working papers to a new series published by the National Association of State Mental Health Program Directors, taking on the question: "What is the inpatient bed need if you have a best practice continuum of care?" In The Role of Permanent Supportive Housing in Determining Psychiatric Inpatient Bed Capacity, Sherry Lerch and Kevin Martone discuss the importance of permanent supportive housing (PSH) as a core intervention in a strong community-based system, and how PSH capacity can reduce the demand for psychiatric inpatient beds. In The Role State Mental Health Authorities Can Play in the Delivery of Integrated Primary and Behavioral Health Care for People with Serious Mental Illness, Including Those with Co-Occurring Substance Use Disorders, Sherry Lerch lays out changes in planning, financing, and procedures that can help SMHAs improve care integration.
TAC Staff in Action
Staff Activities
TAC Managing Director Marie Herb and Senior Associate Liz Stewart both led workshops at the HOPWA Institute in Tampa, a HUD event focused on housing's role in ending the HIV epidemic; Associates Ashley Mann-McLellan and Douglas Tetrault and consultant Naomi Sweitzer helped design and deliver a series of intensive, day-long trainings for direct services staff in the Supportive Services for Veteran Families program; Executive Director Kevin Martone has been named to the board of the National Association for Rural Mental Health, and attended its annual conference in San Diego; Mayra Pabon, our Administrative Assistant, attended the Boston Center for Independent Living's celebration lunch for Transition Internship Program participants, including TAC summer intern Hawo Osman; Senior Consultant Lisa Sloane, Associate Ellen Fitzpatrick, and Production/Design Associate Adriana DePalma put the finishing touches on a series of "HUD PRA 811 Success Stories" which went live mid-month (see above); Senior Associate Jim Yates co-presented on "Supportive Services for Veteran Families and Beyond" at the Kansas Housing Conference; and Senior Associate Gina Schaak represented TAC at a "Massachusetts Housing Day" at the State House, organized by the Citizens' Housing and Planning Association.
Staff Transitions
We're happy to announce that Jennifer Ingle has joined TAC as an Associate with TAC's human services group. Jenn brings expertise in program evaluation, stakeholder engagement, and policy related to long-term services and supports, and has many years' experience working directly with elders and people with psychiatric disabilities. We are also delighted to welcome Madison Tallant, a graduate student in social work at Boston College, as a TAC intern with our housing team this year.
September 2017: Making a Healthier Workplace for Everyone
MANY PEOPLE WITH SERIOUS MENTAL HEALTH CONDITIONS (SMHCs) need employment income in order to meet their basic needs and live independently in the community. However, challenges both in finding and in keeping a job have kept unemployment and underemployment rates high in this group. “Supported employment,” an evidence-based practice in which service providers help a person find and hold a competitive job, is a valuable resource. Yet even people who benefit from this approach may struggle to attain financial self-sufficiency if their jobs are low-paying or part-time, especially if these positions don't qualify them for workplace benefits like health insurance, disability insurance, and paid time off.
Sustainable Employment
While employee readiness is important, there are many other factors that can boost job longevity and success. By prioritizing these alongside employee readiness, we can create the conditions for long-term, sustainable employment. For instance, the potential value of social capital, or “the collective value of social network connections and resources that generate instrumental, informational, and emotional support,” has not yet been fully recognized. Strong social capital increases job satisfaction and retention for everyone — including employees with serious mental health conditions.
Organizational Social Capital
In addition to personal social capital, which includes the support and encouragement of close family, partners, and care providers, the role of organizational social capital is also critical. Organizational social capital refers both to positive social relations with supervisors and coworkers, and to policies and practices that promote healthy workplace norms — features strongly influenced by the culture of each specific workplace. Even an employee with the best job coach in the world can be derailed by an unfriendly or toxic work environment in which they experience discrimination, stigma, unclear expectations, or a murky and difficult process for requesting reasonable accommodations. As these are areas over which employers, not employees, have the most control, organizational leaders who want to help workers with SMHCs to thrive and contribute should consider introducing specific changes in workplace culture.
A Better Workplace for All
So how can employers impact workplace culture to support people with SMHCs? Usually, this shift is facilitated by changes in the areas of onboarding, supervision, and the process for requesting and providing accommodations. Wellness initiatives and SMHC awareness trainings can give all staff good information and tools to meet challenges as they arise, while making the workplace better for everyone. To support these initiatives, employees’ assumptions must be addressed, with leaders taking the important step of directly challenging stereotypes of people with SMHCs as incapable or helpless. Managers will need first to educate themselves, and then to follow up by issuing directives, changing job expectations, offering trainings, and endorsing the efforts of successful supervisors.
People with serious mental health conditions who don’t receive benefits or subsidies need jobs that pay a living wage and that provide crucial workplace benefits. Unfortunately, too many with SMHCs struggle to find and keep such jobs in workplaces unequipped to support their natural resilience. Fortunately, the changes that can lead to sustainable employment for people with SMHCs — such as individualized and regular supervision, efforts to reduce stigma, and efficient approaches to reasonable accommodation — are readily achievable. Furthermore, these shifts are likely to benefit organizations overall.
Future Access blog posts will take a closer look at important elements in sustainable employment. Meantime, find out about TAC's trainings for behavioral health organizations and agencies working with peer specialists.
August 2017: News, Resources, and Happenings at TAC
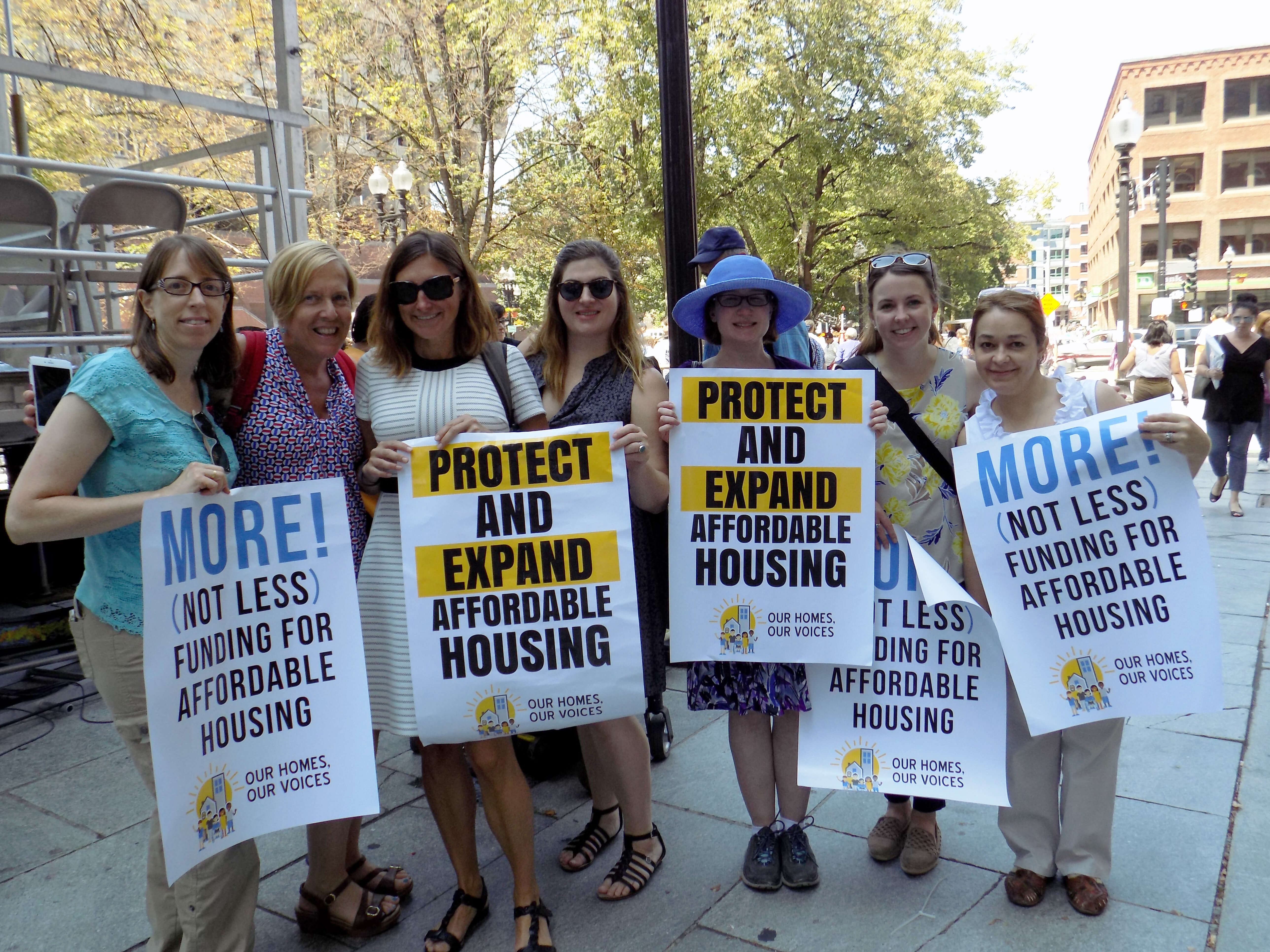
Our Homes, Our Voices — No Housing Cuts!
TAC staff headed over to historic Faneuil Hall a few weeks ago, where we joined hundreds of other housing and disability rights advocates, subsidized housing residents, and community leaders to tell the federal government: NO CUTS TO HOUSING! The Boston rally was organized by our friends at the Citizens' Housing and Planning Association in coordination with events held around the country. Check out our Facebook photo album to see a few of the speakers we cheered for, and take a look at #OurHomesOurVoices on Twitter for a national snapshot.
New Action Plan Launched for Permanent Supportive Housing in North Carolina
Many of the strategies in North Carolina's 2017 Permanent Supportive Housing Action Plan are based on a Permanent Supportive Housing Assessment with Recommendations to Comply with the Olmstead Settlement produced by TAC. The shared vision for permanent supportive housing in North Carolina connects people to affordable, integrated, and supportive housing by leveraging resources and collaborating with all levels of government and private agencies.
CMS Helps States to Foster Community Living Opportunities
The Centers for Medicare and Medicaid Services (CMS) has announced a second round of the State Medicaid-Housing Agency Partnerships track in its Medicaid Innovation Accelerator Program (IAP). The goals of this track are to develop public and private partnerships between state Medicaid and housing systems and to support states in creating detailed action plans that foster community living opportunities for Medicaid beneficiaries. TAC is part of the IAP technical support team that will work from August 2017 through April 2018 with eight states: Alaska, Massachusetts, Michigan, Minnesota, Nebraska, Texas, Utah, and Virginia. Visit the CMS website to learn more.
TAC Staff in Action
STAFF ACTIVITIES
TAC Associates Phillip Allen, Ellen Fitzpatrick, and Ashley Mann-McLellan and Senior Associate Melany Mondello attended the National Conference on Ending Homelessness in Washington, D.C. last month, with presentations by Phil on the SSVF System Assessment Toolkit and by Ashley on the intersection of housing, mental health, and substance abuse; Jon Delman, Senior Associate, was an invited participant in SAMHSA's expert resource meeting on "Advancing Behavioral Health Treatment & Recovery through Technology" and led a workshop on "Fighting for our Livelihoods: Developing Job Opportunities for Economic Self-Sufficiency" at the National Empowerment Center's Alternatives Conference; Associate Lauren Knott and other experts helped out at a forum for SAMHSA's 10 Youth Homelessness Demonstration communities; Executive Director Kevin Martone described the importance of affordable housing for people with disabilities at a #NoHousingCuts Congressional reception organized by Monarch Housing Associates of New Jersey; Kevin also spoke on the role of community-based mental health services and housing in reducing reliance on emergency and inpatient care in his address to mental health authority leaders gathered at the National Association of State Mental Health Program Directors' annual conference; and Senior Consultant Jim Yates was promoted to the rank of Colonel in the Army National Guard - congratulations, Jim!
STAFF TRANSITIONS
We are happy to welcome Hawo Osman as a TAC intern this summer. Hawo is a rising senior at Medford High school and joins us through the Boston Center for Independent Living’s Transition Internship Program.
July 2017: News, Resources, and Happenings at TAC
TAC Scholarship Helps Launch a Teacher, a Social Worker, a Nurse, and a Chef
We are delighted to introduce this year’s recipients of the second annual Day-O'Hara Community Integration Scholarship. This cash award, given in honor of TAC co-founders Steve Day and Ann O'Hara, is intended to help individuals with disabilities in the Greater Boston area to realize their educational and professional goals.
Eddie Shields is currently employed as a teacher’s assistant and was referred to us through the Boston Center for Independent Living. He will use the scholarship money towards courses to obtain his Associate’s Degree in early childhood education.
Kayla Wilson is a Long-term Support Services Coordinator at the Boston Center for Independent Living. Kayla has discovered that her true passion is to assist individuals from both the medical and social points of view simultaneously, and plans to use the scholarship money towards prerequisite courses for nursing programs.
For two years, Lisa Jones has volunteered weekly to serve meals to elders in need. Lisa was referred to us by the Transformation Center, and will use the scholarship money for a post-bachelors program in gerontology — moving her closer to her goal of attaining a Master’s degree in social work or human services so that she can work in a wraparound program to help elders stay in their own homes.
Silvaria DeSilva has a background in nursing, but has recently discovered a love for cooking. She recently graduated from Pine Street Inn’s food service training program, and will use the scholarship money for cooking classes and to buy the supplies and materials she’ll need as a professional chef or caterer.
Best of luck to all, and thanks to the partner organizations that helped us connect with these inspiring individuals!
Successfully Employing and Financing Peer Specialists in Behavioral Health
The inclusion of peer providers on behavioral health care teams can significantly improve client engagement and outcomes, including symptom reduction, improved self-esteem, and community integration. Yet behavioral health providers sometimes struggle to maintain a strong peer workforce — leading to diminished productivity and increased stress for all staff. In TAC’s new training for behavioral health providers, managed care organizations, and state/county behavioral health authorities, participants will learn how to introduce appropriate supports and key shifts in workplace culture to promote both peer job success and stronger organizations overall.
TAC Staff in Action
Staff Activities
In June, Managing Director Marie Herb and Senior Associate Gina Schaak served as volunteer “Ambassadors” at Boston’s Third Surge to End Chronic Homelessness (read all about it!); TAC Associate Ashley Mann-McLellan presented on “Using Data to Improve Outcomes and HUD’s System Performance Measures” at the All Home Annual Conference in Seattle, WA; Kevin Martone, Executive Director, recorded a webinar for Foothold Technology on "Navigating the World of Medicaid for Supportive Housing Services"; and at the National Coalition for Homeless Veterans conference, TAC Associate Douglas Tetrault co-presented with our partners from Abt Associates on how to assess the components of a crisis response system and develop improvement strategies.
June 2017: Putting the Pieces Together
Even though “Bill” showed up right on time for Boston’s Third Surge to End Chronic Homelessness, he told me that he "thought it was going to be stunt, a lot of talking but nothing to show for it.” But when Bill left the building — some seven hours after I greeted him as his assigned ambassador for the day — he had plenty to show for his efforts: a doctor and an appointment, an insurance provider, and best of all his own apartment. It was clear that this was no stunt but an incredible collaboration between the Commonwealth of Massachusetts, the City of Boston, and lots and lots of providers and volunteers.
Behind the Scenes
In many ways, an event like this is just plain old common sense: Bring together all the players — MassHealth/Medicaid, Social Security, the Boston Housing Authority, the Metropolitan Boston Housing Partnership, accountable care organizations, homeless service providers, housing navigators, and the people who need what all of them have to offer — to resolve the barriers that have kept Boston's chronically homeless individuals from finding and keeping housing. But that view is just like looking at the face of the watch and not seeing all the intricacies that hide behind it.
Led by the Massachusetts Department of Elder Affairs and Boston's Department of Neighborhood Development, the Boston Surge was the product of months of detailed planning and collaboration. Data was shared between MassHealth and homeless shelter and outreach providers, and matched to identify individuals over age 50 who had been living on the streets or in homeless shelters for a year or more or who had experienced homelessness several times over the past few years. Some of these individuals were currently on Medicaid while others had previously been, but were no longer active. For the Third Surge, 124 individuals were invited and encouraged and supported to participate. Meanwhile, the Boston Housing Authority and the Metropolitan Boston Housing Partnership looked through their portfolios of housing units and subsidies to identify available housing resources. An individualized "passport" with potential options of health care and support services was created for each person before the event.
The Big Day
Finally, on the day of the Surge, the teams arrived. Representing Social Security, MassHealth, the Housing Authority, service providers, and accountable care organizations, they brought computers, printers, and a determination to get the job done. Ambassadors (all volunteers like myself) were each connected to one "guest" and walked them through the process. The day was busy, chaotic at times, but filled with an energy and a collective sense of will to get people housed. There were no photo ops, no speeches — there was too much work to do.
More than half of the people experiencing chronic homelessness who had been invited — a strong turnout — came to the event. Bill and I got to know one another over breakfast. A Boston native, he fell on hard times two years ago, lost his housing, and had been living in a shelter ever since. On the spot, we got Bill's social security documentation printed out. We met with several providers from senior care organizations, and he signed up for health services, supportive services, and a primary care physician.
Next, we filled out the Boston Housing Authority application and waited while staff reviewed Bill's criminal background records and other eligibility requirements. We sat outside the room and smiled each time we heard clapping indicating that someone had received a housing unit. Then it was Bill's turn. He was told he was eligible, and then got to pick a housing development that met his needs. The applause was for him this time. He sat there just saying over and over, "I thought this was going to be a stunt, I can't believe it!"
Real Results
Boston’s Third Surge to End Chronic Homelessness produced impressive results. Forty-two elders left this one-day event with offers of apartments, while another seventeen have strong linkages to housing after a few more steps. MassHealth was able to re-enroll or upgrade coverage for 12 participants. And 62 elders are now engaged with supportive services to help them stabilize their health and housing for the long term.
The best news is that Boston's model can easily be replicated. No big hero is required — or even stunt doubles. All it took to make it happen was the commitment of key individuals and agencies, along with plenty of hard work. I’m proud of Boston for coming together to end chronic homelessness, and I know your community can do it too.
June 2017: News, Resources, and Happenings at TAC
Propelling Innovation to End Youth Homelessness
TAC consultants have been criss-crossing the U.S. this spring to help strengthen local youth homelessness prevention efforts. In Washington's Seattle/King County, our TA is an integral part of the Youth Homelessness Demonstration Program, a HUD initiative awarded to ten communities. So far, we've worked with Seattle/King County on flexible system design, engaging a Youth Advisory Board, compiling promising practices from across the country, analyzing data to measure the need for housing and services, creating landscape scans of current housing and service inventories, and developing continuous improvement strategies the community can use to evaluate and learn from implementation. Once the planning process wraps up in July, our focus will shift to creating an implementation "road map" for community stakeholders and providing training and capacity-building to Seattle/King County agencies working to end youth homelessness in their community. Learn more about TAC's TA with programs serving children and youth.
Sharing Strategies for Successful Community Integration
From May 1-2, HUD Section 811 Project Rental Assistance grantees from 25 states — including both housing and service providers — joined TAC staff members and officials from the Department of Housing and Urban Development (HUD) and the Centers for Medicare and Medicaid Services (CMS) in Washington, DC. Participants in this TAC-organized initiative shared successes and insights from their experiences implementing PRA to expand integrated supportive housing opportunities for extremely low-income people with disabilities.
TAC Staff in Action
STAFF ACTIVITIES
Policy Advisor Francine Arienti and TAC consultant Naomi Sweitzer were invited by the Vermont Youth Homelessness Prevention Plan Committee to present on federal/state resources and models of state plans around the country; Senior Associate Jonathan Delman gave the keynote address at Employment Matters! (annual conference of the Massachusetts Association of People Supporting Employment First); Jon's article on "Employer-based Strategies to Increase Employment Rates for People Living with Serious Mental Illness," co-authored with Senior Consultant Lynn Kovich and Executive Director Kevin Martone, has been published in Psychiatric Rehabilitation Journal; Associate Ashley Mann-McLellan hosted a community planning meeting in Denver to help advance the city's strategy on ending veteran homelessness; Ashley also met with HUD Youth Homelessness Demonstration Project grantees and TA providers at the CSH Supportive Housing Summit in May; and Associate Douglas Tetrault presented on "Community-wide System Assessment and Improvement" at the National Coalition for Homeless Veterans conference, while Senior Consultant Jim Yates presented on "Using Federal Fair Housing Guidance to Reduce Access Barriers to Housing" at NCHV's pre-conference Housing Summit.
POSITION AVAILABLE
TAC is seeking a Senior Associate/Consultant with expertise in behavioral health and Medicaid. Read the full description and application information.
April 2017: Fulfilling the Vision of Fair Housing Month
APRIL MARKS THE 49th ANNIVERSARY of the passage of the Fair Housing Act. Yet people with disabilities were not covered by this transformative legislation until twenty years later. In passing the 1988 amendments, Congress at last embraced a national commitment to end the unnecessary exclusion of people with disabilities from the American mainstream.
Unfortunately, that commitment remains unfulfilled. In its 2017 report on national discrimination trends, the National Fair Housing Alliance (NFHA), a consortium of more than 220 nonprofit fair housing organizations, state and local civil rights agencies, and individuals from across the United States, reports that “As has been the trend over the past several years, housing discrimination against persons with disabilities continued to make up the majority (55.1 percent) of housing complaints investigated in 2015 across the board, with a total of 15,332 instances reported.”
A press release from U.S. Department of Housing and Urban Development (HUD) Secretary Ben Carson has proclaimed this year’s fair housing theme to be Fair Housing Equals Opportunity, “highlighting equality in housing as a foundation upon which aspirations can be achieved and affirming the Fair Housing Act’s ongoing role in confronting housing discrimination.” We welcome HUD’s continued commitment to fair housing and encourage the Secretary to maintain the agency’s robust support for these critical activities:
Enforcement
HUD must continue to prosecute housing discrimination against people with disabilities actively — whether that discrimination takes the form of new construction that is not physically accessible or a property’s policies and procedures that exclude people with invisible disabilities such as mental illness, brain injury, or HIV/AIDS. The NFHA data also indicates how important it is that HUD continue to fund local fair housing organizations that work directly with those impacted by exclusion and discrimination.
Training
New professionals enter the affordable housing field every year. Whether helping an architect who must sort out multiple state and federal requirements or a property manager who needs to master the subtleties of reasonable accommodation, HUD can play a supportive role, both directly and by funding community organizations that provide technical assistance.
Collaboration
HUD’s continued collaboration internally (e.g. HUD Fair Housing staff working with staff from Public and Indian Housing or Community Planning and Development), across federal agencies (e.g. HUD issuing joint statements with the Department of Justice), and with outside parties (e.g. Consortium for Citizens with Disabilities meeting regularly with HUD’s Assistant Secretary for Fair Housing) is vital to ensuring fair housing for people with disabilities.
Fair housing enforcement, training, and collaboration can help to create equal opportunity. However, actively and affirmatively furthering fair housing (AFFH) — as the Fair Housing Act requires — is vital to success. We urge HUD to commit to continued implementation of the AFFH final rule, including training and technical assistance activities. Disability issues are not yet adequately addressed in HUD’s technical assistance model but with commitment, we know HUD will get there. Let’s make next year’s 50th anniversary of the Fair Housing Act a real celebration.
April 2017: News, Resources, and Happenings at TAC
Appealing to Affordable Housing Developers in Boston
When affordable housing developers and service providers collaborate, new possibilities open up for people who have been homeless to make the transition to being long-term, successful tenants. TAC, together with the Boston Department of Neighborhood Development and Mayor Marty Walsh, led a convening at City Hall on April 13 to foster such partnerships — and specifically to encourage the implementation of homeless veteran and “move on” preferences in affordable housing properties. Speakers described the key role that prioritizing vacant units for populations such as homeless veterans and supported housing residents plays in Boston’s efforts to end homelessness. TAC Associate Ashley Mann-McLellan, who helps communities across the U.S. build public-private partnerships to implement homeless preferences in HUD-assisted housing, explained how developers can adopt homeless preferences with the support of service providers to ensure successful results for everyone: new tenants, their neighbors, and property staff.
TAC Staff in Action
Senior Associate Jon Delman has joined the board of the Association for People Supporting Employment First – MA chapter; Senior Consultant Sherry Lerch presented to the leadership of AbbeHealth in Cedar Rapids, IA on ways to maximize the effectiveness of permanent supportive housing; Associate Ashley Mann-McLellan led a two-day, customized workshop on Housing First for providers in Long Island, NY, and a training on property owner engagement for organizations serving homeless veterans in Denver, CO; Executive Director Kevin Martone taught a class this semester to 3rd and 4th year medical students at Tufts University Medical School, on “Mental Health Systems and Public Health”; at the National Council for Behavioral Health Conference in Seattle, WA, Senior Consultant John O’Brien presented on Medicaid strategies for supportive housing and co-led a recovery housing workshop; Senior Policy Advisor Lisa Sloane and Associate Ellen Fitzpatrick — plus a film crew — headed to Maryland, Minnesota, and Louisiana to work on our forthcoming videos about the HUD 811 Project Rental Assistance program; Senior Consultant Jim Yates presented on “National Trends in Supportive Housing” at the Housing Leadership Group Summit in Albuquerque, NM, and on the National Housing Trust Fund at the National Low Income Housing Coalition’s Legislative Forum in Washington, DC; Jim has also been conducting strategic planning sessions in communities that are part of HUD’s Vets@Home initiative; the TAC Supportive Services for Veteran Families team was instrumental in planning and delivering eight regional meetings for SSVF grantees and their community partners, as well as — together with key partners at Abt Associates — eight locally driven community meetings around the country to help Continuums of Care in their efforts to end veteran homelessness.
News, Resources, and Happenings at TAC: March 2017
Access: The TAC Blog is Launched!
With the addition of Access to TAC’s website, our senior consultants are now able to contribute their unique perspectives from the intersection of affordable housing, health care, and human services policy. Posts so far have included John O’Brien on “The Next Frontier: Care and Service Integration for People with Substance Use Disorders” and Kevin Martone asking “Can States Take On the Fiscal Responsibility that Federal Policymakers Are About to Hand Them?” Watch your email for monthly post alerts.
A New “Practice Profile” on In-Home Therapy
In the fall of 2015, the Children’s Behavioral Health Initiative (CBHI) Knowledge Center, in collaboration with MassHealth, began an extensive effort to develop a “practice profile” for providers of in-home therapy to Massachusetts children and youth receiving publicly funded behavioral health services. After conducting a literature review and a series of workshops with stakeholders, CBHI drafted the new resource and engaged TAC to help produce the final version. Publicly available, the In-Home Therapy Practice Profile offers in-home therapy providers easy-to-use guidance on best practices in cultural relevance, risk assessment and safety planning, engaging natural supports, and other key areas.
TAC Staff in Action
Staff Activities
Senior Associate Liz Stewart participated in the inaugural Winter Walk across Boston to end homelessness; Liz and Associate Lauren Knott joined a panel on “Improving Systems in Balance of State and Regional CoCs” at the National Alliance to End Homelessness’ Annual Conference on Ending Family & Youth Homelessness.
Staff Transitions
We’re happy to welcome Phillip Allen as a new Associate on the TAC housing team. Phil is helping Supportive Services for Veteran Families (SSVF) grantees and communities to develop and implement effective programs.
March 2017: Two Olmstead Settlement Agreements Resolved, but the Future of Community Integration is Unclear
DEPENDING ON WHOM YOU ASK, an Olmstead settlement agreement can be a blessing or a curse. While the parties typically agree on the principle affirmed by the U.S. Supreme Court — that people with disabilities should live in the most integrated setting possible — costly housing markets and complex service delivery systems are formidable barriers to this goal. More than 15 years after the Supreme Court's landmark Olmstead decision, states still struggle to serve people with disabilities in integrated settings.
Delaware and New Jersey are two states that have recently resolved their Olmstead settlements, achieving significant reforms though years of dedicated effort — Delaware's settlement was originally signed in 2011 with the U.S. Department of Justice, while New Jersey's was signed in 2009 with Disability Rights New Jersey and the Bazelon Center for Mental Health Law.
Thanks to the successes of these states in substantially attaining the outcomes required by their agreements, thousands of people with serious mental illness now have the opportunity to live in integrated community settings. What is perhaps most impressive is that a substantial part of the system reform accomplished by New Jersey and Delaware occurred during the great recession (2007 to 2009) and the following period of slow economic recovery.
Getting Results
Delaware and New Jersey both offer good examples of what is possible when states focus on community integration for people with mental illness and other disabilities.
A U.S. Department of Justice press release describes some of Delaware’s most significant gains. The state reduced the number of bed days in the Delaware Psychiatric Center by 47.2 percent. The number of Medicaid-eligible Delawareans receiving community-based services has increased by 92 percent since the United States began its investigation. The state has seen the growth of a strong peer and self-advocacy movement that is now incorporated into its entire service system. Two statewide mobile crisis teams and a crisis walk-in center divert 70 to 90 percent of the individuals they engage away from hospitalization and criminal justice interaction and toward community-based services.
As a press release from Bazelon details, New Jersey’s settlement also brought about important changes. Between 2005 and 2016, New Jersey invested nearly $104 million in services and rental assistance for Olmstead-related activities. The state also established a $200 million special needs housing trust fund, and created nearly 1,500 new permanent supportive housing units through capital and rental assistance. New Jersey’s state psychiatric hospital census was reduced by a third, patients’ average length of stay went down, and one state hospital was closed — changes that allowed state hospital operating funds to be reinvested in community supports. New Jersey created a Medicaid benefit to fund community support services for residents of supportive housing, and leveraged additional Medicaid money with investments in community-based services.
Both Delaware and New Jersey used their Olmstead settlement agreements as a driver for change, embracing a community integration platform to guide them toward significant behavioral health system reform. These states recognized that without sustainable system reform and new resources, counting numbers to achieve settlement targets wouldn’t bring about the changes needed to serve people with serious mental illness effectively.
Commitment to Olmstead in a Changing Landscape
Across the country, Olmstead stakeholders are raising questions about the future of community integration for people with serious mental illness and other disabilities. Doubt surrounds the capacity and motivation of states to tackle Olmstead in the years ahead; the commitment of the Department of Justice to focus on Olmstead as strongly as it has in the past; and the ability of protection and advocacy organizations to hold states accountable.
Changes to the Medicaid landscape at the federal level could put at risk the types of benefits coverage that makes community integration work for people with disabilities. Looming cuts to non-mandatory discretionary budgets, such as HUD housing assistance programs, may further jeopardize the ability of states to support community integration.
The Department of Justice has been instrumental in the movement toward community integration, enforcing Olmstead by leading investigations, entering into settlement agreements in several states, and intervening in support of class actions. If the Department shifts its attention to other priorities established by the Trump administration, individuals with serious mental illness and other disabilities will be left without civil rights enforcement at the very time when loss of benefits could place them at greater risk of institutionalization. Many state protection and advocacy agencies, as well as legal services organizations, have the authority to bring class action lawsuits on behalf of people with disabilities, and these groups may be called upon to step up their efforts.
Complying with Olmstead will become increasingly difficult if federal policy and budgetary changes reduce support to states in the near future. Federal cuts currently under consideration would put people with mental illness and other disabilities at greater risk of institutionalization and homelessness due to thinner benefits and services and reductions to the rental assistance that can make housing affordable. Our February blog post on budget impacts explained the challenges states will face in making resources available to meet federal requirements. Nevertheless, it is states that are on the hook to ensure that individuals are served in integrated settings.
Community integration mandates in the Olmstead decision, Title II of the Americans with Disabilities Act, and Section 504 of the Rehabilitation Act are still the law, regardless of fluctuations in federal enforcement and support. Furthermore, serving individuals with disabilities in integrated, community-based settings is good, cost-effective policy. With these facts in mind, states should continue to design and implement Olmstead plans that build sustainable, system-wide improvements. The benefits — to individuals, communities, and all who recognize the value of true integration — are well worth the challenges.
February 2017: Can States Take On the Fiscal Responsibility that Federal Policymakers Are About to Hand Them?
A FEW WEEKS AGO, I had the opportunity to explain to a roomful of congressional staffers the profound impact that a repeal of Medicaid expansion would have on individuals with substance use disorders - and on the systems that serve them. In the questions that followed, an underlying theme was evident: Would lost Medicaid revenue and other federal resources be replaced by state funds to pay for such services? This issue has far-reaching implications for all of our nation's safety net programs. Both my current work with state systems across the country and my experience as a former state commissioner of behavioral health make clear to me that states are in no position to absorb the transfer of fiscal responsibility they are about to receive from federal policymakers.
Systems Work Better Together
In every state, there are vulnerable populations whose complex challenges require coordinated solutions that use federal and state funding. In recent years, awareness has grown in both the health care and affordable housing communities of the positive outcomes to be attained by leveraging these resources together. State Medicaid directors have become educated on the costs to their programs of individuals with chronic health conditions who are homeless, at risk of homelessness, or living in substandard housing. Likewise, affordable housing leaders have learned that lack of access to health insurance, and especially to integrated behavioral and primary health care services, jeopardizes housing stability. States are becoming sophisticated in their use of interventions that build on this new understanding, such as supportive housing - an approach that combines affordable housing assistance with wraparound supportive services. Such states have increasingly demonstrated cost savings in their systems.
The availability of federal funding has afforded states the opportunity to improve the lives of millions of children and adults. The option to expand Medicaid through the Affordable Care Act (ACA) allowed states to increase access to care for populations with many health needs, create better health care delivery systems, and save taxpayer dollars. Federal funding was the incentive needed for 31 states and the District of Columbia to expand coverage, while states that did not expand Medicaid still rely on significant federal support to operate their traditional Medicaid programs. Federal housing assistance programs have been a critical resource for millions of seniors, people with disabilities, and people living on very little income - though a significant gap remains between available assistance and need.
Shifting the Burden to States
The imminent repeal of Medicaid expansion and the ACA, and proposals to convert Medicaid to a block grant or per capita program, threaten millions of people's access to health care, with disproportionate consequences for vulnerable populations. While these changes will create significant savings for the federal government, states will in turn experience both immediate and long-term pressures to fill the void - allegedly in exchange for more control and "flexibility." Under a block grant plan previously proposed by former House Budget Chair and Health and Human Services Secretary nominee Tom Price, the Medicaid and Children's Health Insurance Program would receive 34 percent less funding in 2025 than under the current federal law.
Decreases in affordable housing assistance resulting from cuts to non-defense discretionary (NDD) programs like those at HUD will disproportionately affect the same populations impacted by cuts in Medicaid. We don't have to look too far back to see how this plays out: the March 2013 sequestration cuts forced state and local housing agencies to decrease the number of households using tenant-based vouchers by more than 80,000. About half of all voucher recipients are seniors or people with disabilities, most of whom live on fixed incomes such as Social Security or Supplemental Security Income (SSI) and rely on Medicaid. In not a single rental housing market in the country can a person with a disability who is living on SSI afford housing at the "fair market rent" determined by HUD. According to the National Low Income Housing Coalition, the United States has a shortage of 7.2 million rental units affordable to extremely low-income renter households. Yet President Trump has proposed a one-percent reduction to NDD each year for the next ten years. Even a simple freeze, suggested by several members of Congress, would result in the defunding of housing vouchers currently used by more than 100,000 families in 2017 alone.
Faced with such a significant loss of federal support, Democratic and Republican governors, legislators, and mayors will have to make some very difficult budgetary decisions. Will these leaders, as many have suggested, find ways to sustain access to health benefits, affordable housing assistance, and social services once federal policymakers shift the financial burden onto states?
Hard Choices
Recent history shows that as resources are squeezed, many states are unable or unwilling to prioritize vulnerable populations. Most Medicaid expansion states were in a position to increase coverage only because of significant federal matching. Without such support, states have generally opted to provide only limited benefits to people who are traditionally ineligible for Medicaid, and several states have established highly restrictive eligibility criteria. Economic downturns can create added challenges for states as tax revenues decrease while unemployment and enrollment in Medicaid increase. According to the U.S. Government Accountability Office (GAO), during the nation’s last recession, Medicaid enrollment grew by 14.2 percent from October 2007 through February 2010. During the same period, total Medicaid expenditures grew nearly 21 percent, from $332.2 billion in 2007 to $401.5 billion in 2010.
To reduce program spending, the GAO noted, states generally make certain changes to their Medicaid programs, such as altering payments to providers, limiting eligibility, eliminating optional services, or reducing the amount, duration, or scope of services covered. Even as need rose, states cut funding for a range of services by 4.2 percent in fiscal year 2009 and an additional 6.8 percent in 2010, according to estimates by the National Association of State Budget Officers (NASBO). In 2011, two-thirds of states cut provider payments, and 18 states reduced Medicaid benefits. The recession of 2009–2012 resulted in losses of over $4 billion from public behavioral health systems across the country, losses from which they have still not fully recovered.
Most states have allocated resources to support housing assistance for low-income populations. A report prepared by the Technical Assistance Collaborative in 2014 indicated that 34 states offer some type of rental assistance or homelessness prevention funds (e.g. security deposits). However, there is wide variation in the number of individuals such programs can support, and program funding tends to fluctuate annually due to state budget pressures. Indeed, a NASBO survey conducted in the fall of 2016 indicated that in 24 states, general fund revenues for 2017 are coming in below projections, the greatest number of states expecting revenue shortfalls at this time in the fiscal year since 2010. Nineteen states reported net mid-year budget reductions in fiscal 2016, a historically high number outside of a recession period.
There is indisputable evidence that the availability of health insurance and access to health care and affordable housing improve people's lives. As lawmakers contemplate dramatic reductions that will hurt people and economically burden states, we find ourselves at a pivotal point. There is little evidence to suggest that state governments can or will assume the financial responsibility offloaded by the federal government under current proposals. Yet, it is state and local budgets that must absorb the preventable economic consequences when individuals engage costly, crisis-oriented health care, correctional, and homelessness systems. Federal policymakers must understand that a cost shift to states under the guise of flexibility and efficiency will have dramatic and unfortunate consequences for vulnerable individuals and their families.
February 2017: Care and Service Integration for People with Substance Use Disorders - by John O'Brien
THIS MONTH, states are submitting proposals to the Substance Abuse and Mental Health Services Administration (SAMHSA), outlining their plans to address the opioid crisis. While the strategies proposed will vary, SAMHSA’s message is clear: the funds it provides must be used to connect individuals to needed services in communities that have been hit hardest by opioids. Time is of the essence, and states have only a few months — lightning speed for most state bureaucracies — to increase access to substance use disorder (SUD) services.
Many states will no doubt use their awards to expand prevention and treatment programs. That’s terrific — enhancing the services that directly address addiction should be paramount. However, it is of great importance that federal and state agencies also ensure the availability of physical health care and long-term services, such as in-home supports, for individuals dealing with addiction. States should take steps to integrate these forms of care into the continuum of SUD services, rather than relegating them to separate systems.
Awareness has never been stronger of the importance of an integrated approach to treating diabetes, asthma, HIV/AIDS, and behavioral health conditions. Data has helped show the impact these health challenges have on people’s morbidity, quality of life, and health care costs, while also revealing that people who have any one of these conditions often have others on the list as well — or are at significant risk for acquiring them.
The good news is that insurers and health care providers recognize the need to coordinate medical, behavioral health, and long-term services. Over the past ten years, Medicare and Medicaid have laid the foundation for developing integrated care models to help tens of millions of Americans — and private sector insurance companies have followed suit. These insurers have learned from the pioneering work of health care providers in integrated care, and are bringing their efforts to scale.
A Good Use of Resources
Much of the energy powering integration efforts in behavioral health has so far been directed specifically toward mental health. As the opioid crisis intensifies, however, private and public insurers are paying increased attention to the impact of substance use disorders on morbidity. Meanwhile, prompted by federal requirements that many insurance plans cover SUDs, insurers have found plenty of data that offers compelling reasons to integrate physical health care, SUD services, and long-term supports.
Individuals with untreated SUDs and co-morbid medical conditions often incur high medical costs. For instance, $3.3 billion was expended in one year on behalf of 575,000 Medicaid beneficiaries with a secondary diagnosis of an SUD — triple the cost for those without an SUD. Two of the top ten reasons Medicaid patients are readmitted to a hospital within 30 days of discharge are SUD-related. Conditions that occur more frequently among individuals with SUDs than in the general population include respiratory issues, skin infections, and suicide.
Other problems related to SUDs are opioid-exposed pregnancies, drugged driving, and increases in Hepatitis C and in some circumstances HIV. Opiate use during pregnancy increased from 1.19 to 5.63 per 1000 hospital births from 2003 to 2009; seventy-eight percent of these births were to women covered by Medicaid. For newborns with Neonatal Abstinence Syndrome (NAS) and their mothers, the post-delivery costs are seismic — $43,000 per child versus $900 per child who does not have NAS.
To succeed fully, integration efforts must also factor in the social determinants of health. Many individuals with SUDs are homeless or have unstable living arrangements, challenges that often render health care needs secondary to the search for affordable and safe housing.
Meeting the Need
For insurers who are ready to introduce or enhance integrated care, the first task is encouraging recognition of the need. This may also be the easiest task, as insurers already have the data to make a strong clinical and business case for integration. The next step is to use the data to be more precise regarding who, what, and where should be the focus of insurers’ attention.
First, who? While some individuals are at elevated risk of acquiring a substance use disorder, others have struggled with addiction for decades. Insurers can’t assume that a one-size-fits-all integration program is sufficient. Using data analytics, we can identify the specific health care, treatment, and recovery service needs of different populations. These results can be used in turn to develop data-informed integration strategies.
Which leads to the question of what models an insurer might implement as part of an integration strategy. Some approaches are well-researched and proven to be effective. For instance, the Screening, Brief Intervention, and Referral to Treatment (SBIRT) model has proven invaluable in assessing an individual’s SUD risk and providing immediate and short-term interventions. Screening and brief intervention should occur in a doctor’s office; if patients have more extensive treatment needs, the doctor can make a referral to an SUD treatment provider who is either part of the same practice or a member of a network of practitioners and organizations specializing in SUD treatment.
For individuals with more intensive SUD treatment needs, models for integration are still developing. Several states have created partnerships between physical health care providers and SUD care providers to increase access to evidence-based treatment, such as medications coupled with counseling. Other insurers have assembled teams of physicians, nurses, licensed SUD practitioners, and recovery coaches to coordinate the health, behavioral health, long-term supports, and social services needed by people with significant health and SUD challenges. Evaluations are underway to measure the effectiveness of these strategies.
And finally, the where. Where does it make sense for insurers to invest in new and existing models of integrated care for individuals with an SUD or at risk of an SUD? Again, the answer is not immediately clear. The models highlighted above are being tested in primary care settings, emergency departments, and the specialty SUD system. Some insurers have been working with health clinics to increase access to SUD medications (which generally must be prescribed by a physician or other health practitioner). Other insurers have invested in placing physicians, nurses, and physician assistants in SUD specialty agencies, creating teams to help the high need/high cost individuals who often engage with this system.
In these times of uncertainty, it makes sense to prioritize the protection of individuals’ access to insurance coverage and treatment services — but this can’t be our only focus. Excellent progress has been made over the past eight years to introduce and sustain integrated care for people with substance use disorders, and to test models that will improve their quality of care while reducing costs. Let’s keep going.
News, Resources, & Happenings at TAC: February 2017
Core Principles for Housing and Health Care Policy: A Statement from TAC
TAC's Board of Directors met on December 8, 2016, to discuss the ways our organization can help ensure that leaders make informed decisions about proposed changes to health care and insurance, affordable housing, social and economic policies, and the other programs that form our country's safety net. On January 10, we issued a statement of the principles that will guide our work and advocacy in the months and years ahead.
Read the full statement.
Educating Congress on the Important Role of Medicaid in Preventing and Treating Substance Abuse Disorders
On January 25, TAC Director Kevin Martone and other panelists addressed some 70 congressional staffers representing legislators of both parties. Organized in partnership with the National Council for Behavioral Health, this event offered lawmakers the opportunity to learn that decreased federal support would have a devastating effect on state substance use treatment systems - and showed them why preservation of coverage for individuals with substance use disorders is crucial.
Melville Charitable Trust Roundtable Highlights Housing Program Progress
Since 2012, HUD has awarded Section 811 Project-based Rental Assistance (PRA) funds to 28 states and the District of Columbia. By establishing state-level partnerships among housing, Medicaid, and human services agencies, these state grantees have been able to develop integrated, affordable, accessible housing opportunities - with access to voluntary supports - for people with disabilities who have extremely low incomes. Under contract with the Department of Housing and Urban Development (HUD), TAC is a provider of TA for these Section 811 PRA grantees. On January 12, TAC facilitated a Melville Charitable Trust-sponsored roundtable event to discuss the demonstration program's progress. The roundtable included participants from six states (MN, NJ, PA, MD, TX, and LA), HUD staff, the National Council of State Housing Agencies, the National Low Income Housing Coalition, and the Center on Budget and Policy Priorities. A lively discussion focused on recommendations to increase access to affordable housing, leverage resources effectively, and identify best practices in service delivery.
TAC Staff in Action
Staff Activities
Associate Ashley Mann-McLellan recently led a workshop for funders in Seattle/King County, WA on how to incorporate Housing First principles into their requirements, contracts, and monitoring processes - and, together with Associate Lauren Knott, conducted a Housing First training for the Cambridge (MA) Continuum of Care;Working with the Supportive Services for Veteran Families (SSVF) program and the U.S. Interagency Council on Homelessness, TAC Associate Doug Tetrault helped plan and facilitate a community meeting for 60 local stakeholders focused on effectively ending veteran homelessness in Orlando, FL; Senior Associate Jon Delman's symposium on "Successfully Employing Young Adult Peer Mentors: From Research to Practice with the Employer Toolkit" has been accepted by the Psychiatric Rehabilitation Association for its 40th annual Wellness and Recovery Summit; Kevin Martone, TAC's Executive Director, spoke at a Congressional briefing this month on "Expanding Access to Care," hosted by the National Council for Behavioral Health; Kevin also spoke at the National Press Club on December 12 as part of the National Governors' Association event "Housing as Health Care: A Roadmap for States"; and in December, Senior Policy Advisor Lisa Sloane presented on Louisiana's Section 811 PRA program at a public workshop hosted by the National Academies of Sciences, Engineering, and Medicine; and Associate Amy Horton and Senior Associate Gina Schaak volunteered at Boston's Homeless Count the night of January 25.
TAC Transitions
Congratulations to Liz Stewart on her promotion to Senior Associate with the TAC housing team!